EMST: Speech Therapy for Parkinson's Disease
Parkinson's disease can affect breathing, swallowing, and speech in ways that are not always expected. Many people notice coughing during meals, changes in voice, or trouble clearing their throat.
Expiratory muscle strength training (EMST) focuses on these changes by strengthening the muscles used for breathing, coughing, swallowing, and speech.
Key Takeaways
Expiratory Muscle Strength Training (EMST) strengthens the breathing muscles that support respiration, swallowing, speech, and cough function, directly targeting airway safety and effective communication.
EMST uses a one-way valve device to strengthen the muscles involved in forceful exhalation, helping improve cough effectiveness, swallowing (dysphagia), and speech in conditions such as Parkinson’s disease, stroke, ALS, and COPD. Adjustable resistance increases the effort required to exhale, similar to strength training for the respiratory muscles.
Clinical research shows that EMST can significantly improve swallowing function and voluntary cough strength, supporting safer eating, a louder voice, and improved quality of life for individuals with neurologic and respiratory conditions.
EMST: Speech Therapy for Parkinson's Disease and Other Neurologic and Respiratory Conditions
How Expiratory Muscle Strength Training Improves Cough Function
Research on EMST for Parkinson's Disease and Other Conditions
What EMST Speech Therapy Programs Look Like for People with Parkinson's Disease
Who Benefits from Expiratory Muscle Strength Training
Frequently Asked Questions About Expiratory Muscle Strength Training
EMST: Speech Therapy for Parkinson's Disease and Other Neurologic and Respiratory Conditions
Expiratory Muscle Strength Training (EMST) is a therapeutic intervention that uses a pressure-threshold device to strengthen expiratory muscles. Stronger expiratory pressure supports clearer speech, safer swallowing, and a more effective cough. Speech-language pathologists trained in these areas use EMST to address respiratory, voice, and swallowing deficits associated with a range of neurologic and respiratory conditions.
Expiratory Muscle Strength Training and Breathing Support
EMST uses controlled resistance during forceful exhalation to strengthen the muscles involved in breathing, airway protection, and cough. During training, an individual exhales into a calibrated one-way valve device set to a specific pressure threshold. This targets the expiratory muscles of the respiratory system as well as muscles involved in airway closure and protection.
Why Breathing and Airway Control Can Change
Neurologic and respiratory conditions, such as Parkinson’s disease, stroke, ALS, and COPD, can affect muscle strength, coordination, and timing. These neurologic and physiologic changes may reduce breath support for speech, weaken cough effectiveness, and compromise swallowing safety. EMST helps improve the physiologic support needed for airway protection, communication, and daily function.
Parkinson's Speech Therapy Techniques
Check out our blog on Parkinson's speech therapy techniques for more information!
How Expiratory Muscle Strength Training Improves Cough Function
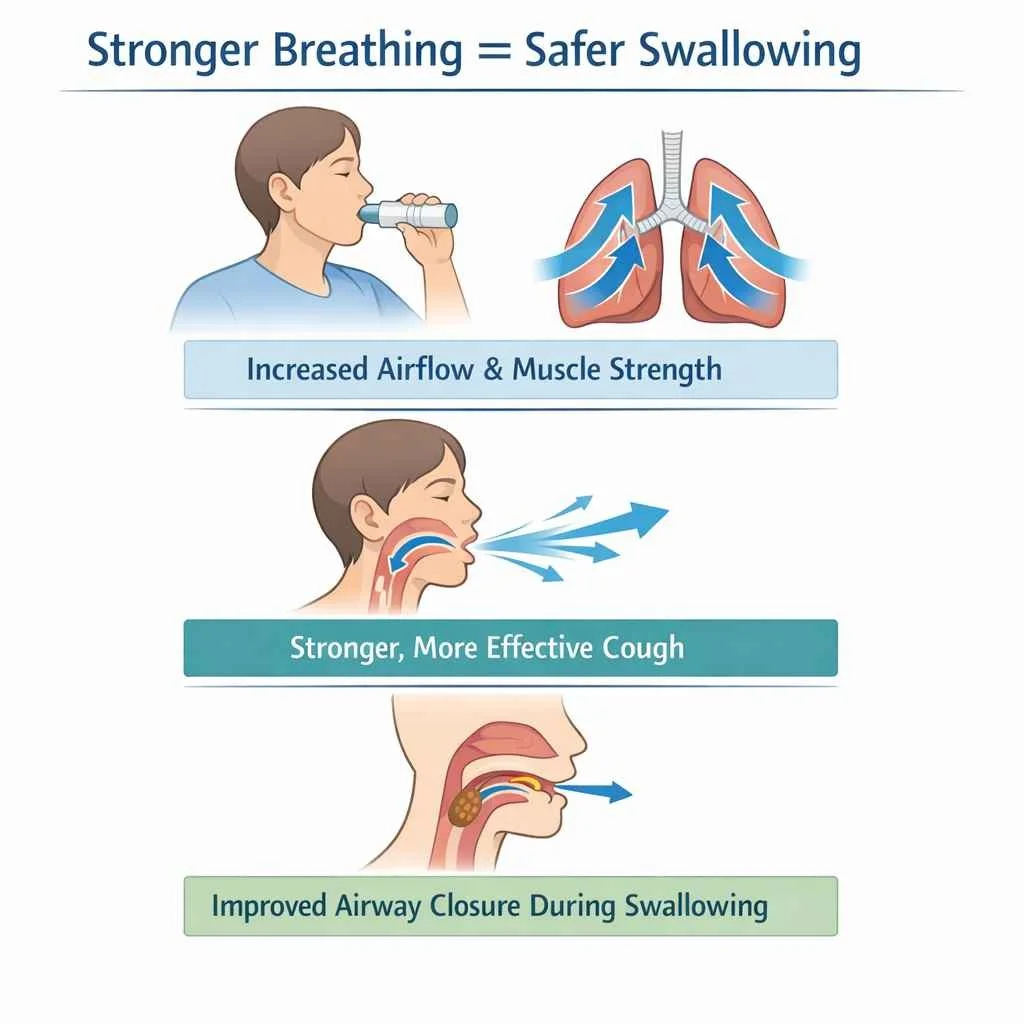
EMST can improve swallowing function and cough strength by increasing expiratory airflow and respiratory muscle strength. Stronger expiratory muscles support airway protection during swallowing, helping reduce the risk of choking and aspiration across neurologic and respiratory conditions.
Swallowing Symptoms and Dysphagia
Swallowing symptoms may include coughing during meals, slowed chewing, or the sensation of food sticking in the mouth or throat. Dysphagia can occur in conditions such as Parkinson’s disease, stroke, ALS, multiple sclerosis, and COPD, raising safety concerns and affecting nutrition and quality of life. EMST targets the muscle systems involved in airway protection to support safer swallowing.
Voluntary Cough and Airway Protection
A strong voluntary cough helps clear food, liquid, or saliva from the airway. EMST increases maximum expiratory pressure, thereby improving cough strength. This added respiratory support helps maintain airway safety during daily activities for individuals with neurologic and respiratory conditions.
Research on EMST for Parkinson's Disease and Other Conditions
Research in neurology and speech-language pathology supports EMST as a non-pharmacologic, exercise-based intervention that can increase maximum expiratory pressure (MEP) and strengthen airway-protective functions such as voluntary cough and swallowing safety. Randomized controlled trials in Parkinson’s disease demonstrate measurable improvements in swallowing safety and cough-related outcomes following structured EMST protocols.
What Research Shows About EMST
Studies show that EMST can help people produce a stronger cough and better protect their airway during swallowing. Research also indicates that improved expiratory strength and airflow may support speech breathing and vocal loudness by providing better breath support for voice production. Participants who complete a guided EMST program demonstrate improved airway safety compared to those who do not receive active training.
University Research and Neurology Collaboration
Much of the EMST research has been conducted by university-based teams in speech-language pathology and neurology. Researchers, including Troche MS, Rosenbek JC, and Okun MS, have examined how expiratory muscle training affects breathing strength, swallowing safety, and cough function, supporting EMST as a structured, evidence-based speech therapy intervention.
What EMST Speech Therapy Programs Look Like for People with Parkinson's Disease
EMST follows a structured training plan under the guidance of a trained speech-language pathologist. Each program is based on evaluation results and individual ability. Consistent practice supports improvement.
Assessment and First Step Planning
A speech-language pathologist completes an assessment of swallowing and speech. Maximum expiratory pressure is measured to properly set the EMST device. This first step guides safe training.
Daily Expiratory Muscle Strength Training Structure
Most programs include five breaths per set and five sets per day. Training usually lasts about five weeks, with regular clinician check-ins. The focus remains on controlled pressure and correct technique.
Who Benefits from Expiratory Muscle Strength Training
Individuals with neurologic or respiratory conditions, such as Parkinson’s disease, stroke, ALS, or multiple sclerosis, who experience changes in swallowing, breathing, or speech may benefit from expiratory muscle strength training. A comprehensive evaluation helps determine whether EMST is appropriate and how it should be incorporated into treatment.
Symptoms That Affect Speech, Swallowing, and Breathing
Symptoms may include coughing during meals, reduced voice volume, frequent throat clearing, or shortness of breath when speaking. These changes can interfere with communication, eating safety, and daily activities.
Clinician Guidance and Safety
EMST should be completed under the guidance of a trained speech-language pathologist. Clinician oversight ensures proper pressure settings, correct technique, and safe progression of the program.
Frequently Asked Questions About Expiratory Muscle Strength Training
1. When is EMST used for Parkinson's disease?
EMST may be used when a person with Parkinson’s disease experiences reduced cough strength, changes in swallowing safety, or decreased breath support for speech. The program uses a pressure-threshold EMST device to strengthen expiratory muscles and is guided by a speech-language pathologist to support airway protection and communication.
2. How long does EMST take?
An EMST program typically lasts several weeks, with short daily practice sessions completed at home. The exact duration and schedule are individualized and guided by a speech-language pathologist based on the person’s needs and response to training.
3. Can EMST help with swallowing problems and choking?
EMST can support swallowing function and reduce the risk of choking in certain cases. Research links EMST to better airway closure. This change can reduce aspiration risk. A speech therapist who specializes in speech and swallowing and is trained to use the EMST device determines whether EMST is appropriate.
4. Is EMST safe for people with Parkinson's disease?
EMST is safe when supervised by a trained clinician. Pressure levels are based on assessment results. Monitoring supports correct breathing technique. This approach protects airway safety.
How Connected Speech Pathology Can Help
At Connected Speech Pathology, we provide remote speech therapy support for individuals with Parkinson’s disease and other neurologic or respiratory conditions. Services focus on communication and voice education, and strategies that support daily function through secure telehealth sessions.
When appropriate, our speech-language pathologists discuss evidence-based approaches such as EMST and help clients understand how breathing, cough, and swallowing changes may affect communication and safety. Speech therapy emphasizes individualized guidance, education, and practical strategies that can be applied in everyday life.
Summary
EMST speech therapy for Parkinson's disease targets breathing, swallowing, and cough deficits through structured training. Research supports its role in improving airway protection and communication. Guided speech therapy can support safer swallowing and stronger cough function.
About the Author
Allison Geller is a communication coach, speech-language pathologist, and founder of Connected Speech Pathology, an international online practice providing professional communication coaching and speech therapy for children, teens, and adults. With more than two decades of experience, she has worked in medical and educational settings, published research on aphasia, and leads a team of specialists helping clients improve skills in public speaking, vocal presence, accent clarity, articulation, language, fluency, and interpersonal communication.