Ways to Improve Speech in Parkinson's Disease
Parkinson’s disease (PD) is the world’s second most common neurodegenerative disease after Alzheimer’s disease, with approximately 10 million people worldwide living with PD. Parkinson’s disease is a progressive neurodegenerative disease that comes with more than about 60 different symptoms.
There are movement and non-movement symptoms. The primary movement symptoms in PD include slowness, impaired balance, rigidity, and tremor. Some non-movement symptoms include memory and cognitive changes, depression, anxiety, sleep problems, and changes to speech, voice, and swallowing.
While 89% of individuals with PD have a speech or voice problem (Logemann et al.,1978) and 45% will develop articulation problems (slurred speech), most do not recognize that they have a speech problem. It is often the caregiver who realizes the change in communication first.
Communication Disorders Associated With PD Can Impact Quality Of Life
When a person has dysarthria, articulation can be imprecise. Hypophonia, which means soft speech, is an abnormally weak voice caused by weakening muscles. Tachyphemia, also known as cluttering, is characterized by an excessively fast speed of talking. Reduced intelligibility can cause frustration during communicative interactions and may result in social withdrawal. Unfortunately, due to these speech changes, others with PD may be perceived as bored or disinterested when they are not.
Dysphagia, also known as swallowing difficulty, can occur. When a person takes a long time chewing or holding food in their mouth for a long time, and muscles become weak and uncoordinated, coughing and choking may occur. A speech pathologist can provide a swallowing evaluation and identify compensatory swallowing strategies to make swallowing easier and safer. This may include suggestions for how to take medications safely. A speech pathologist may also make suggestions for diet modifications to make swallowing safer. This evaluation is typically conducted on an outpatient basis at a medical center.
Cognitive Challenges may include difficulty with concentration, planning and sequencing tasks, word-finding, expressing thoughts, following conversations in large groups, understanding the emotional meaning of a conversation, changing topics quickly, and losing ‘train of thought’.
Voice- The Basics
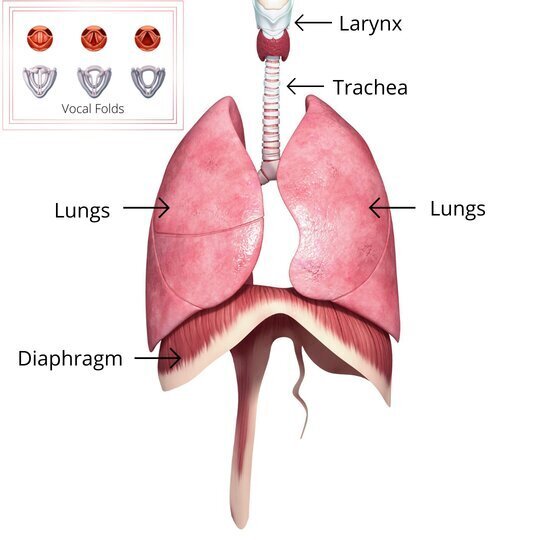
Respiration, or breath support, is also known as the “power source” to produce voice. When we speak, the air is initially brought into the lungs (inhalation). The air is then expelled from the lungs (exhalation). It passes through the trachea (windpipe) and arrives in the larynx (throat), where the vocal folds are located. The vocal folds vibrate, creating a vibration or “buzz.” The articulators (lips, teeth, tongue, and jaw) turn the “buzz” into speech.
Voice- What Happens In PD?
Individuals with PD experience neural damage and a reduction in the release of dopamine. This can lead to poor breath support or reduced respiration. Less breath support means changes to vocal quality, loudness, and pitch. The voice may be hoarse, breathy, and quiet. Reduced loudness makes it difficult for the individual to be heard in regular conversation and when speaking over the crowd noise. The pitch of the voice is what controls the variation of the highs and lows of the voice, also known as “inflection.” When the voice lacks liveliness, it can be perceived as boring and can lead to misunderstandings during a conversation.
Treatment Strategies: High Effort Exercise
Since the automatic system isn’t working well for those with PD, speaking requires a high level of effort. People with PD need to exercise their bodies and voices every day. Many drug therapies help some of the symptoms, but over time, unfortunately, symptoms progress. Research shows that there is great value in exercise in PD because exercise can improve brain functioning (neural plasticity) and may slow disease progression.
Speech therapy has been shown to help people with PD who experience speech difficulties. Most speech therapy for people with PD aims to improve loudness, rate, or inflection (pitch variations). Treating speech difficulties in Parkinson’s disease should always be customized to the individual’s needs and the challenges they are experiencing.
The following are suggested programs for high-effort speech therapy for individuals with PD:
The Lee Silverman Voice Treatment Program (LSVT)
LSVT Loud is delivered over 16 sessions during a 4-week period. The program emphasizes intensive vocal and physical effort for maximal plasticity (Kliem & Jones, 2008). This focus on effort is thought to override the altered, slow muscle movements and recalibrate new vocal effort and loudness levels, particularly as the disease progresses.
LSVT Loud is one of the most widely used programs and has been tested and shown to have positive outcomes for persons with PD, with improvements that can last up to two years. LSVT must be delivered by a clinician who is certified in the program.
Some “unexpected”, positive outcomes of LSVT Loud include improvements in articulation, swallow, rate of speech, facial expression, and speech motor stability (Spielman, et al. 2002; El-Sharkawi, 2002; Spielman et al., 2003; Kleinow et al., 2001; Liotti et al., 2003).
Expiratory Muscle Strength Training (EMST)
EMST works to build up the muscles that push air out of the lungs for speech. This can result in more syllables per breath and a stronger voice for people with PD. A simple resistance device called “EMST” or “The Breather” is used to build strength. The device should be used under the direction of a speech pathologist. It is reusable by a single patient, is very cost-effective, and requires daily practice. The speech pathologist can adjust the device setting as the patient improves.
SpeechVIVE
The SpeechVIVE is a medical device that the individual with PD wears that feeds background noise into the ear, prompting the person to talk louder. The device is set to elicit a 3-5 dB increase in SPL. The individual with PD wears the device each day for 2-8 hours during communicative situations. The speech pathologist resets the device as the person improves.
SpeakOUT
Parkinson’s Voice Project SPEAK OUT!® is a two-part speech therapy approach to help those with PD regain and maintain speaking abilities. The “Speak Out” program is followed by group therapy called “The Loud Crowd.” The “Speak Out” program consists of 25 lessons laid out in a specialized workbook that includes speech, voice, and cognitive exercises. The program focuses on speaking with “intent.” NCBI research shows the results last up to a year and are comparable with other programs. Speech pathologists delivering the program should be trained specifically in “Speak Out.”
Other Beneficial Communication Programs and Devices
Visual Feedback (Apps)- There are several different apps available that can provide visual cues to the person for loudness, articulatory precision, rate, and intonation. Examples include ORAI, Speeko, and Speak Up For Parkinson’s. A dB Sound Meter, such as Decibel X, can also be helpful in measuring loudness.
Voice Amplifiers- A speech pathologist can help you determine if a voice amplifier is suitable for you. Voice amplifiers typically include an amplifier worn around the waist with an attached head mic, such as the Chattervox.
Speech Generating Device (SGD)- A speech-generating device is a communication aid in which an electronic communication system is used to supplement or replace speech or writing for individuals with severe speech impairments. The individual can press a button or activate a switch to play back a recorded message.
Speech Therapy Can Have A BIG Impact for Individuals With PD
Participation in speech therapy can have a multitude of benefits. Improved communication skills can build confidence and lead to a return to social life. With new confidence, individuals with PD may be more likely to talk to family, speak with large groups, engage in casual conversation and speak in noisy settings.
Getting Treatment
Treatment can be delivered using telepractice (online speech therapy). It can also be delivered in a clinic, hospital, or rehab center.
Telepractice: The Benefits
At Connected Speech Pathology, we use telepractice to connect with clients. We have been providing speech therapy using online speech therapy for years. Research shows it is as effective as in-person treatment, and our clients have all been very happy with the ease and effectiveness of this method for delivering speech therapy.
Obtaining treatment via telepractice offers several benefits, including reduced or eliminated travel time, reduced fatigue, increased access to Speech-Language Pathologists for those living in rural areas, no waiting in waiting rooms for extended periods, and decreased exposure to illness/viruses/germs.
Telepractice also reduces mobility challenges and allows for the generalization of treatment skills into the natural environment. To connect with your speech pathologist via telepractice, you need a computer with a camera and microphone, and an internet connection.
How To Get Started With Speech Treatment
Ask your doctor for a referral and a prescription for a speech evaluation and treatment. Then contact us to set up an appointment. We will provide you with simple instructions to connect with us online.
Difficulty communicating is socially isolating, frustrating, and can even make it difficult to express simple wants and needs. This is why it is so important to address the individual communication needs of people with PD in the most effective ways possible. If you or someone you know would benefit from communication treatment, please contact us.
About the Author
Allison Geller is a communication coach, speech-language pathologist, and founder of Connected Speech Pathology, an international online practice providing professional communication coaching and speech therapy for children, teens, and adults. With more than two decades of experience, she has worked in medical and educational settings, published research on aphasia, and leads a team of specialists helping clients improve skills in public speaking, vocal presence, accent clarity, articulation, language, fluency, and interpersonal communication.